Edward Chang is a neurosurgeon, scientist, and a pioneering leader in functional neurosurgery and brain-computer interface technology, whose work spans the operating room, the research lab, and the engineering bench to restore speech and movement for patients who have lost these capabilities. In this episode, Edward explains the evolution of modern neurosurgery and its dramatic reduction in collateral damage, the experience of awake brain surgery, real-time mapping to protect critical functions, and the split-second decisions surgeons make. He also discusses breakthroughs in brain-computer interfaces and functional electrical stimulation systems, strategies for improving outcomes in glioblastoma, and his vision for slimmer, safer implants that could turn devastating conditions like ALS, spinal cord injury, and aggressive brain tumors into more manageable chronic illnesses.
Timestamps: There are two sets of timestamps associated with the topic list below. The first is audio (A), and the second is video (V). If you are listening to this podcast with the audio player on this page or in your favorite podcast player, please refer to the audio timestamps. If you are watching the video version on this page or YouTube, please refer to the video timestamps.
The evolution of neurosurgery and the shift toward minimally invasive techniques [A: 2:30, V: 1:17]
- There’s so much Peter wants to talk about with respect to Edward’s career, the field of neurosurgery today, and how the bounds are really being pushed
- Neurosurgery remains a little bit of a black box
What were the typical problems that would’ve presented to a neurosurgeon in the latter part of the 19th century, and what were the tools they had at their disposal?
- We’re speaking after the development of anesthesia
- It’s a very small group of physicians that are taking care of fairly severe indications
- It’s a rarefied field that requires very long training in addition
If we go back 100 years, we’re talking about the era of Harvey Cushing who’s considered the father of modern neurosurgery
- That was a clear inflection point in the history of medicine, in the history of neuroscience, and the history of neurosurgery
- It was really the beginning of what we’d call the modern neurosurgery
- Cushing was a really an astute observer, an incredibly technically skilled surgeon, and also an incredible internist
- He diagnosed some of the first pituitary tumors and the effects of those on endocrine function
- This was the era of modern tools of craniotomy
- Opening the skull to get access to brain tumors and everything followed since then
⇒ The main categories of neurosurgery have to do with tumors, the vascular system (which are aneurysms and strokes and blood clot), the spine, and then probably the most recent one is the one we call “functional”
- Functional neurosurgery has to do with understanding the functions of brain circuit but also intervening to change how they work using deep brain stimulation or other ablation methods
- Harvey Cushing would be credited for the development of the electrocautery
- It’s hard to imagine you could operate without one of those
- It’s the key of controlling bleeding in any surgery, but particularly in the brain (it’s a tricky thing)
Harvey Cushing was just the starting point of modern neurosurgery
Then there’s Wilder Penfield
- He who was an American but really did some incredible work in creating the Montreal Neurological Institute, and that was really the beginning of what we would consider modern epilepsy surgery
- Surgeries that are designed to stop people from having seizures
- He popularized this thing that we all learn in medical school called the homunculus [shown in the figure below]
- It’s this picture of the little man there and essentially the part of our brain that controls every muscle in our body and how it’s laid out in that particular part of the brain
- It’s something that we all learn
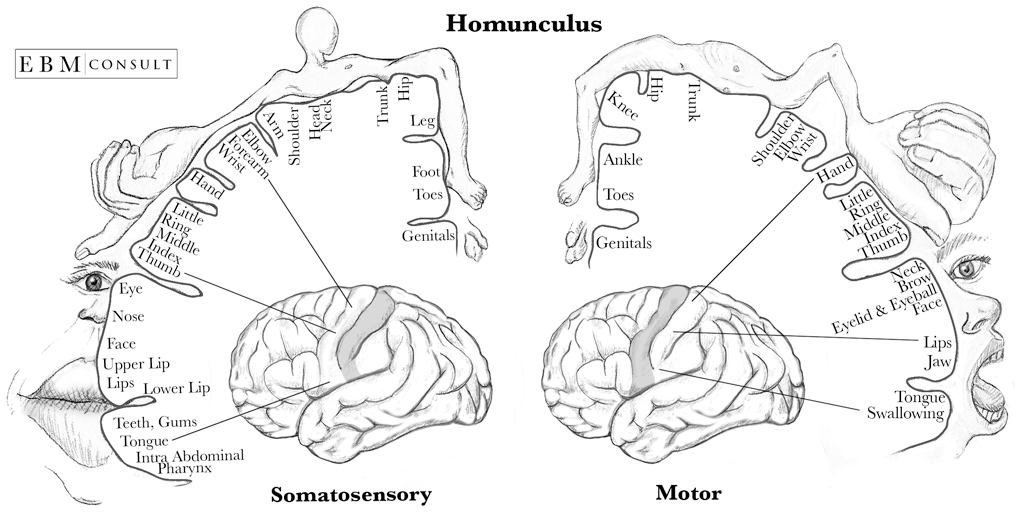
Figure 1. Homunculus. Image credit: Evidence-Based Medicine Consult
- He was also a brilliant scientist who helped us understand some of the basic things that we know about language and, from a technical perspective, really popularized and developed the concept of awake brain surgery
- Awake brain surgery is really something that’s captivated Edward since medical school and what he specializes in now
Fast forward to the ‘70s and ‘80s, what was state of the art 40, 50 years ago with respect to vascular management, oncologic management of masses in the brain relative to today?
What were the plateaus in technology?
- Some of the things that we do now are almost identical to the way that Cushing did it over 100 years ago, and then some of it is radically different
- One of the workhorse surgeries that we do is called a craniotomy
- That basically means where you remove a piece of bone temporarily (you replace it at the end of the procedure) to access something like a brain tumor that’s in the frontal or a temporal lobe
- That’s still being performed today and still really indicated
- But where we are now, there’s ways of using laser probes through very small incisions to get to deep targets in the brain to ablate them
- There are ways of now even using focus ultrasound that can be targeted to specific nuclei in deep parts of the brain in order to control someone’s tremor for example
This is what we would consider a relatively non-invasive approach to do a neurosurgery ‒ so things have changed radically
One other area where we have seen tremendous disruption is in the vascular neurosurgery field
- Back in the ‘80s and ‘90s, you’d have a large craniotomy and incision probably about 7-9 inches long, removal of a piece of bone and then using an operative microscope to dissect down to the deepest parts where the blood vessels are coming to fix, let’s say, an aneurysm
- An aneurysm is essentially a ballooning of a blood vessel that when it ruptures, can be fatal
- That is a lot of what Edward trained on
⇒ Nowadays, 90% of those procedures are now done through a catheter in the groin that’s visualized
- We put coils into the aneurysms to help secure them
- We can now do stents ‒ a huge change now being able to retrieve and dissolve clots that are causing acute severe strokes
Probably the most dramatic things that we’ve seen
- Someone comes in, not able to talk, paralyzed on half side of the body
- In the old days, we would just give some medications keeping our fingers crossed that that would work
- It rarely worked; it was really the minority of cases that it helped
- Nowadays, there’s a much bigger fraction of patients where you can put the device in and retrieve the stroke
- These are really game-changing things when someone can go home the next day after such a huge thing
We’re starting to see things like stroke become more like heart attacks
- The cath labs are not just treating heart attacks but they’re also treating what we call “brain attacks” or strokes
- Some things are relatively similar to 100 years ago and then some things have just been totally changed
If 30 years ago, a neurosurgeon was doing a craniotomy virtually every time they were addressing a pathology, today it might be less than half the time?
- Yeah, that’s right
- Peter notices that’s not a dissimilar parallel to what we see in other parts of surgery
- He was just talking to a vascular surgeon a couple of weeks ago who finished his training around the time Peter did and Peter asked, “How many open surgical procedures are you doing?”
- Peter was talking about AAAs and all sorts of Fem-Pops and things like that
- He said it’s virtually all done with stents… even carotid arteries, the whole thing
- Peter was really blown away at how little they’re operating now in an open sense
What’s happened with surgery is the force of evolution is guiding us towards things that are more minimally invasive, with less collateral damage to get to the targets and get people back to life sooner
“It’s a very exciting time, actually, to be in medicine with all this technology that’s coming on board.”‒ Edward Chang
Glioblastomas: biology, current treatments, and emerging strategies to overcome its challenges [A: 10:45, V: 10:58]
- Whenever Peter thinks of the brain, he thinks of GBMs (these awful tumors)
Tell folks what a GBM is, and why a GBM is truly one of the cancers that gives cancer a bad name
{end of show notes preview}
Would you like access to extensive show notes and references for this podcast (and more)?
Check out this post to see an example of what the substantial show notes look like. Become a member today to get access.


